The emerging digital twin technology, which was originally purposed for the manufacturing and aerospace industry, has also found its footing in the healthcare sector because of its many practical applications.
A market analysis report by Grand View Research points out that the market size of digital twin in healthcare “was estimated at USD 902.6 million in 2024 and is projected to reach USD 3.55 billion by 2030, growing at a CAGR of 25.9% from 2025 to 2030.”
By leveraging real-time data integration, advanced analytics, and virtual simulations, digital twin technology has the potential to enhance patient care, enable predictive analytics, optimize clinical operations, and facilitate training and simulation. In addition to offering personalized treatment plans based on gathering patient data from various sources, predictive analytics and preventive interventions are made possible by machine learning algorithms of digital twins, allowing for early detection of health risks and proactive interventions.
Further, digital twins can analyze workflows and manage resource allocations, leading to streamlined processes and improved patient care. Yet another application of digital twins in healthcare is the creation of a safe and realistic but virtual environment for healthcare professionals to enhance their skills and practice complex procedures.
Nevertheless, while the digital twin in healthcare is heralding a digital health transformation, its underlying architecture—the sophisticated interplay of data systems, models, sensors, analytics, and clinical workflows—is often less understood.
In this post we shall take a look at what’s behind the scene—how digital twin architectures are designed, deployed, and maintained within the medical ecosystem.
What Is Digital Twin in Medicine?
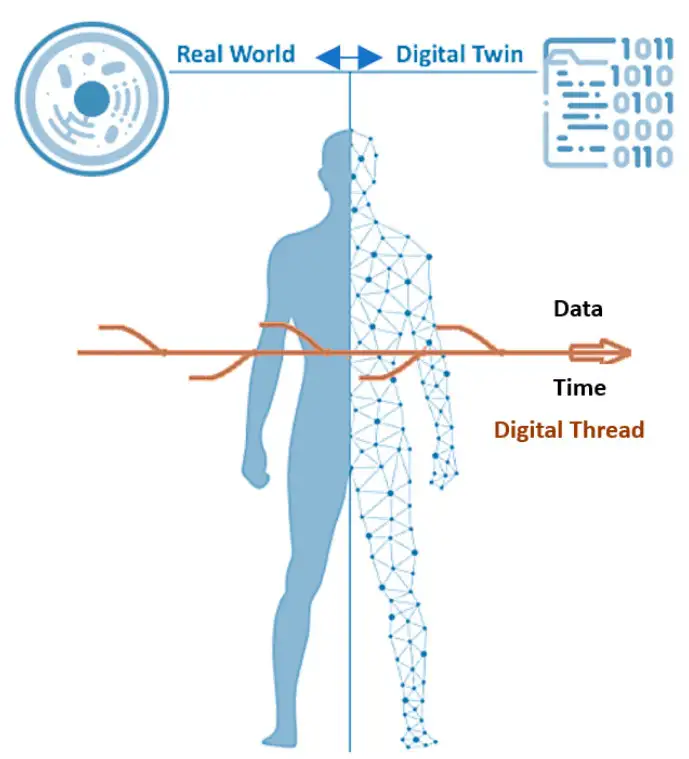
Conceptually, a digital twin in healthcare could be a digital replica or representation of a physical object (healthcare IoT sensors or machines like X-ray machines), a process (managing staff rotation, billing, etc.), or even an individual organ or an entire patient. It is a virtual model (data plus algorithms) with special features not found in traditional models and simulations, one that dynamically pairs the physical and digital worlds and leverages modern technologies, such as smart sensor technology, data analytics, and artificial intelligence (AI) in order to detect and prevent system failures, improve system performance, and explore innovative opportunities.
The most defining characteristic of digital twins is the bi-directional links between the physical entity and its corresponding twin in the digital domain through which live and uninterrupted data is shared, which is the vital element for the entire system.
Needless to say, unlike a machine, an assembly line, or a factory, replicating a human body, an emergency room, or a hospital ecosystem is extremely complex, but thanks to scientific knowledge and extensive simulation capabilities, it is now possible to construct digital twins for modelling different functions such as the biophysical systems or protein structures of the human body or the aspects of an entire hospital ecosystem.
Source: PMC PubMed Central
And however complex it is, a typical digital twin system consists of three main components: the physical entity (source) in the physical environment, the digital representation of the physical entity in the virtual space, and connections between the two—data and information flowing between the physical and digital replica.
Benefits of Digital Twins for Hospitals
Digital twins in medicine are used to:
- Predict disease progression
- Simulate treatment outcomes
- Optimize surgical planning
- Monitor chronic conditions
- Personalize drug dosing
- Improve device performance
- Hospital operations optimization
- Drug development and trials
To make this possible, a robust architecture that integrates data acquisition, preprocessing, modeling, simulation engines, analytics layers, and end-user interfaces is needed, all while ensuring safety, privacy, and regulatory compliance.
What Is a Medical Digital Twin Architecture?
Different applications call for different architectures of digital twin in medicine, but most include the following six core layers:
Data Acquisition Layer: Feeding the Digital Twin
Data forms the foundation of any digital twin, and this data needs to be accurate, timely and multimodal, captured from various sources like wearables, machines, systems etc.
Types of Data Collected
- Electronic Health Records (EHRs): Diagnoses, prescriptions, lab reports, vitals
- Medical Imaging: MRI, CT, ultrasound, PET
- Wearables and Sensors: Heart rate, oxygen saturation, movement, glucose readings
- Genomics and Biomarkers: DNA sequencing, proteomics, metabolomics
- Clinical Staff Inputs: Treatment updates, notes, observations
- Medical Devices: Pacemakers, infusion pumps, ventilators
- Environmental Context: Smart room sensors, bed occupancy
- Historical Data: Previous admissions, medication history
Real-Time vs. Batch Data
Digital twins may be:
- Real-time, ingesting continuous streams (ICU twins, cardiac monitoring)
- Near-real-time, updating every few minutes or hours
- Batch-updated, refreshed after new imaging or lab results
Devices and Data Sources
Examples:
- Wearables (Fitbit, Apple Watch, Dexcom)
- Implantables (pacemakers, neurostimulators)
- Hospital equipment (MRI scanners, ventilators)
- Healthcare IoT sensors (body temperature patches, smart beds)
This layer demands uninterrupted connectivity and is crucial for the proper functioning of the digital twin. It is a must to ensure mechanisms such as Bluetooth Low Energy (BLE), Wi-Fi, NFC, and HL7/FHIR.
Integration & Interoperability Layer: Making Data Usable
Gathering data is only half the battle won, but the challenge remains that healthcare data is notorious for its fragmented nature as it comes from various sources. To build a functional digital twin, information must be:
- Standardized
- Harmonized
- Mapped to clinical ontologies
Key standards and protocols followed to get this done include:
- HL7 and FHIR for EHR interoperability
- DICOM for imaging data
- LOINC for lab tests
- SNOMED CT for clinical terminology
- IEEE 11073 for medical device communication
Also, to format the data and get rid of any other anomalies, the following procedures are followed:
- De-duplication
- Normalization
- Error correction
- Format conversion
- Removal of outlier or corrupt data
Finally, virtualized digital twins can query data from distributed systems on demand rather than centralizing all data physically.
The role of a robust integration layer is to ensure that the digital twin receives clean, complete, and contextually meaningful data.
Data Processing & Storage Layer: The Digital Twin’s Brainstem
Now that data is gathered and formatted, it is now sent for processing, where it is:
- Cleaned
- Validated
- Transformed
- Encrypted
- Stored
Data Lakes and Warehouses
Digital twins often use hybrid architectures that include:
- Cloud data lakes for raw/unstructured data
- Data warehouses for structured clinical data
- Healthcare-specific cloud environments (AWS HealthLake, Google Health Data Engine, Azure Health Data Services)
Stream Processing
Real-time processing engines:
- Apache Kafka
- Apache Spark Streaming
- Flink
These frameworks support the continuous updates needed for real-time medical twins, such as ICU patients.
Semantic Layer
A semantic layer translates raw data into clinically meaningful entities, such as:
- Blood glucose rising
- Risk of sepsis detected
- Heart rate variability decreasing
Data Storage Considerations
Storage must support:
- High volume (e.g., imaging datasets)
- High velocity (ICU monitor streams)
- High variety (structured + unstructured)
This layer functions as the central data backbone for all modeling and analytics tasks.
Modeling & Simulation Layer: Building the Digital Twin
This is the heart of the digital twin architecture, where data transforms into models that simulate physiology, diseases, devices, or ecosystems of its real-world counterpart. We’ll consider a virtual patient here.
Types of Models
- Physiological Models: Mathematical, biomechanical, or computational biology models simulate organ systems like cardiac electrophysiology, respiratory mechanics, tumor growth, etc.
- Machine Learning & Deep Learning Models: These models uncover patterns, predict risks, and evaluate likely patient outcomes.
- Physics-based Models: Used in surgery planning and device performance evaluation.
- Hybrid Models: Combining domain physics and data-driven ML models creates more accurate, resilient twins.
Multi-scale Modeling
Digital twins merge:
- Cellular level (genes, proteins)
- Tissue level (organ structure)
- Organ systems
- Whole-body physiology
- Environmental context
This multi-scale capability sets digital twins apart from traditional healthcare simulations.
Model Calibration
To ensure accuracy, models are:
- Aligned with patient baselines
- Updated with new data
- Re-calibrated during treatment changes
Continuous Synchronization
The core requirement here is that the virtual twin evolves as the patient evolves.
Analytics & Intelligence Layer: Generating Insights
The analytics layer translates the twin’s data and simulations into actionable insights.
Predictive Analytics
Models estimate:
- Future heart events
- Rate of disease progression
- Surgical risks
- Drug response
- ICU deterioration
Prescriptive Analytics
Recommends clinical actions:
- Drug dosages
- Ventilator settings
- Physical therapy intensity
- Lifestyle changes
Optimization Engines
Used in hospital twins:
- Staffing optimization
- Resource allocation
- Equipment scheduling
- Patient flow management
AI-driven Decision Support
The intelligence layer feeds dashboards, alerts, and clinician tools.
In modern architectures, LLMs (Large Language Models) are increasingly used for:
- Summarizing twin insights
- Translating predictions into clinical language
- Answering clinician prompts
- Automating documentation
This makes the digital twin interpretable and usable by busy medical professionals.
Clinical Application and Interface Layer: Where Humans Interact
The digital twin becomes a practical solution at this stage.
User Types
- Clinicians (doctors, nurses, specialists)
- Radiologists
- Surgeons
- Hospital administrators
- Researchers
- Patients (limited visualizations)
User Interfaces
- Real-time dashboards
- 3D anatomical visualizations
- Mobile apps
- Surgical planning software (AR/VR)
- ICU command centers
- Predictive risk scoring interfaces
Workflow Integration
Successful twins fit into clinical workflows:
- EHR plugins
- Clinical decision support integration
- Mobile alerts
- Visualization during surgeries
- Treatment planning consultations
Human-in-the-Loop (HITL)
Clinicians remain essential for:
- Reviewing AI output
- Overriding recommendations
- Updating patient conditions
- Providing contextual knowledge
Digital twins augment, not replace, medical expertise.
Now that is the basic framework of a typical medical digital twin architecture, but surrounding these layers are two additional components that sustain the ecosystem:
- Security, Compliance, & Governance Framework
- Twin Lifecycle Management & Monitoring
Let’s look at how these layers work.
Security, Compliance, and Governance Framework
As a digital twin in healthcare deals with highly sensitive clinical, imaging, behavioral, and device-generated data, security is of utmost priority. A robust framework ensures that every data flow—from acquisition to analytics to real-time simulation—remains secure, compliant, and ethically governed.
Core Security Requirements
A modern medical digital twin must incorporate:
- End-to-End Encryption: Protects data in motion and at rest across hospitals, cloud platforms, and analytical engines.
- Tokenized Data Exchange: Minimizes the handling of raw patient identifiers, reducing breach risk.
- Role-based Access Control (RBAC): Ensures only authorized clinicians, researchers, or systems access specific data sets.
- Zero-trust Architectures: Every request is continuously verified—no implicit trust within networks.
- Multi-factor Authentication (MFA): Adds an additional layer of user identity protection.
Compliance Standards
To ensure legality and data protection, digital twin implementations must adhere to global and regional regulations:
- HIPAA: Protects patient health information in the United States.
- GDPR: Regulates personal data processing and cross-border transfers in the EU.
- ISO 27001: Provides a structured framework for managing information security.
- FDA Guidelines: Apply to device-driven or predictive digital twins connected to regulated medical devices.
Ethical Considerations
Beyond legal compliance, ethical AI design ensures fairness, transparency, and patient agency:
- No Bias in Training Data: Prevents systemic inaccuracies or unequal treatment in predictive models.
- Patient Consent: Ensures individuals have control over how their digital twin data is collected and used.
- Twin Explainability: Supports interpretable AI outputs that clinicians can understand and trust.
- Transparency in AI-driven Insights: Requires clear documentation of how predictions or recommendations are generated.
A strong governance framework integrates security, compliance, and ethics to ensure that medical digital twin technology remains secure, trustworthy, and aligned with patient rights and clinical standards.
Twin Lifecycle Management: Keeping the Digital Twin Alive
A digital twin is a dynamic system—it evolves as the patient, hospital workflow, and medical knowledge change. Effective lifecycle management ensures the twin remains updated, accurate, safe, and clinically useful.
Continuous Model Updates
Digital twins require regular and timely updates to stay aligned with real-world patient states. For this, you need to:
- Retrain ML models with new patient data to prevent drift
- Recalibrate physiological parameters as health conditions shift
- Integrate new clinical insights from research or updated guidelines
Performance Monitoring
Monitoring ensures the twin’s predictions and simulations remain trustworthy.
- Drift alerts when data patterns shift
- Sensor health checks to detect faulty or missing signals
- Accuracy tracking across model versions and patient cohorts
Scaling Digital Twin in Healthcare Systems
Hospitals must support twins for thousands of patients across high-volume, multi-site environments. This can be made possible through cloud-native architectures—with microservices, containers, and auto-scaling—enabling elastic scaling, resilience, and efficient resource use.
Conclusion
Digital twins are redefining the future of medicine by bringing together real-time data, advanced analytics, and patient-specific modeling. Their true potential is unlocked when they are continuously updated, monitored for performance, and integrated seamlessly with clinical workflows. As hospitals scale these systems across departments and patient populations, strong lifecycle management and a reliable AI backbone become essential.
This is where DeepKnit AI adds value. We support healthcare providers, MedTech companies, and research teams with comprehensive services—ranging from AI solutions and hybrid model development to EHR/device integration, data and workflow automation, drift detection, and compliance-aligned deployment. Our team ensures that your digital twin ecosystem remains accurate, scalable, and clinically reliable over time.
To explore how DeepKnit AI can support your digital twin initiatives, you can book a consultation, request a technical demo, or share your project requirements directly with our team. Let your digital health transformation start today—with the right intelligence, architecture, and expert partnership powering it.